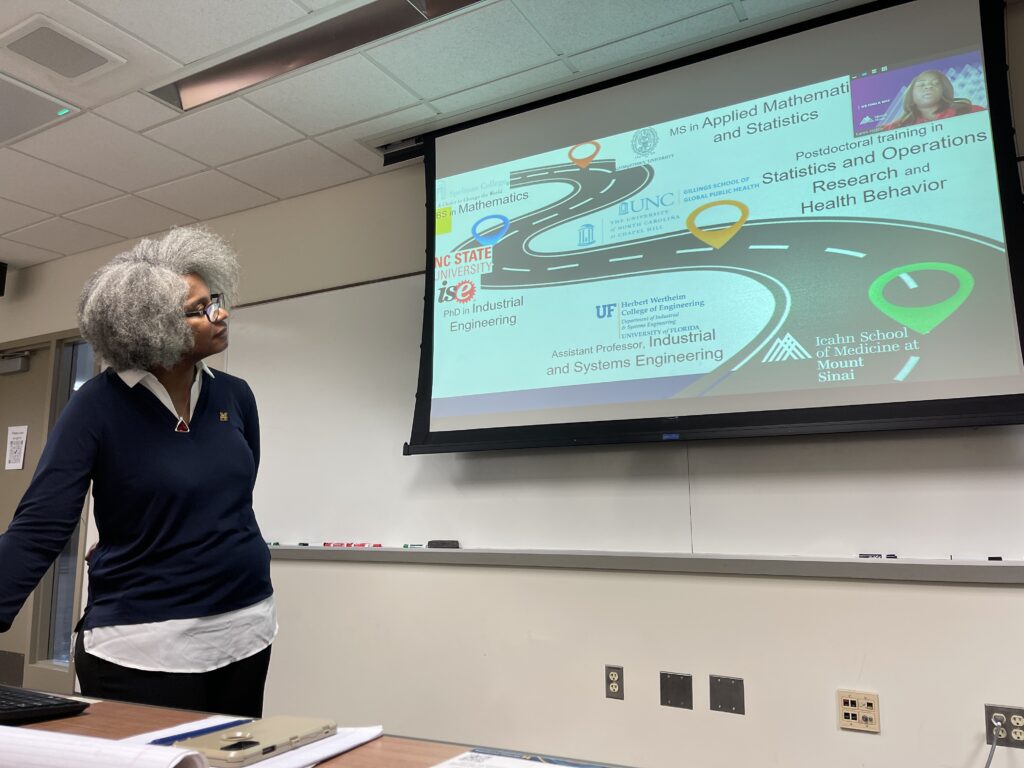
On November 27th, the Providing Better Healthcare Through Systems Engineering seminar series welcomed Julie Simmons Ivy, PhD, MS, the University of Michigan’s Industrial and Operations Engineering Department Chair. She arrived to speak about the significant disparities in health outcomes for birthing people. Students, faculty, staff, clinicians, and community members gathered to discuss the causes and potential solutions to this problem.
“I’m not going to give you a presentation…we are going to have a discussion,” Ivy opened.
Before diving into the topic of maternity disparities, Ivy highlighted her identity as an industrial engineer, sharing, “I think of the world through systems and connections,” and that she often asks herself, “We can do this better. How can we do this better?”
Modeling a better world
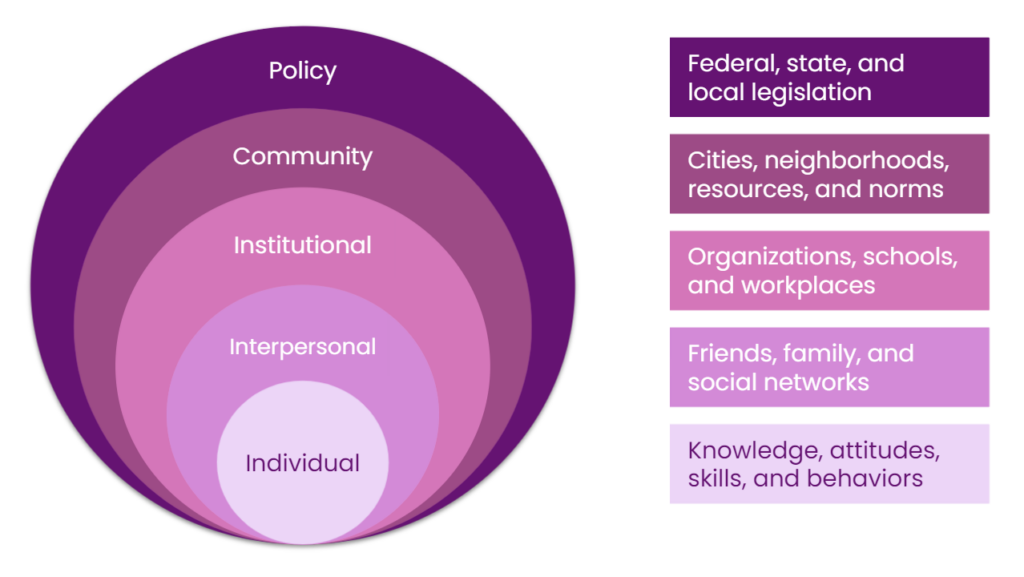
Ivy utilizes human centric decision modeling to inform her work in the sectors of health, hunger relief, and education. This fundamentally involves refusing to ignore the systems in which people live: “It’s really not just about the individual, but it’s about the environment in which they are existing,” said Ivy. She also utilizes the socio-ecological model, which acknowledges that there is no public policy that can be employed free from community, organizational, interpersonal, or individual influences or impacts. This bidirectional model can—and should—directly impact how changemakers think about disparities.
In addition to human centric decision modeling and the socio-ecological model, Ivy employs stochastic, Markov, and Bayesian models as her defining perspectives for bettering systems of all kinds by “[personalizing] solutions to the needs of the individual.”
Ivy’s recent operations research
In partnership with North Carolina State University, Drexel University, MedStar Health, Christiana Care Health System, and Mayo Clinic, Ivy has conducted and published research through her project entitled Sepsis Early Prediction Support Implementation System (SEPSIS). Sepsis, the body’s inflammatory response to infection that goes into overdrive, is a leading cause of death around the world and the second most costly condition to treat by hospitals. This research involved creating a stochastic process that could then be used to predict sepsis, intervene earlier, and reduce sepsis-related mortality.
The second project Ivy shared—Satisfying Households in Areas with Food Insecurity with a Network for Good (SHARING), done in partnership with North Carolina State University, North Carolina Agricultural and Technical State University, and the University of Alabama—is ongoing. Ivy and her collaborators work with food banks, food pantries, and other hunger relief organizations to efficiently prioritize food preferences for community members experiencing food insecurity in both rural and urban areas, all the while avoiding food waste as much as possible. This project is ongoing and will continue for the next several years.
Relation to maternal mortality work
Similarly to Ivy’s work on the SEPSIS project, researching and improving outcomes for birthing people is greatly stochastic: pregnancy is a long and often-changing process, and what works for a patient at one point in time will often not work for them at another point in time. Labor progression, in particular, varies substantially from patient to patient. Further, Ivy shared that “One of the most interesting things about birth is that there are two patients, and those two patients can be having very different outcomes, and the decisions can impact them differently. There’s not a real metric for how you can combine their utilities, actually.”
Ivy then introduced her collaborator, Karen Hicklin, PhD, MS, who joined the conversation via Zoom. Hicklin currently works for the Department of Population Health Science and Policy at the Icahn School of Medicine at Mount Sinai. There, she employs her expertise in applied mathematics, statistics, operations research, and health research within Women’s Institute and the Cancer Institute.
Hicklin and Ivy next spoke about decision-making within the personalized space of maternal health, specifically about the disparities existing around maternal morbidity and mortality.
Investigating the root causes of maternal health disparities
Despite being the wealthiest country in the world, the U.S. has the highest rate of maternal mortality amongst all similarly resourced countries. These numbers only increased since the onset of the pandemic. Further, Black women are three times as likely to die from labor complications. Access-related issues as a result of racist practices like redlining, the frequent dismissal of Black women’s pain, and weathering (the compounded physical toll that bigotry takes on individuals with marginalized identities) are largely to blame for these disparities. Indigenous patients are also more likely to die in childbirth, having seen the largest jump in deaths since 1999 than any other racial demographic.
One birthing practice that considerably varies in both prevalence and outcome? Cesarean sections.
Though common, Cesarean sections—or C-sections—are major abdominal surgeries. Birthing people who need C-sections yet don’t receive them can lose their lives; birthing people who don’t need C-sections yet do receive them can also lose their lives
“That’s why we want to make sure we use it when we should,” said Ivy, “but we don’t accidentally want to overuse it.” It’s not that this potential for overuse is on the horizon, however; it’s real and it’s here.
It is medically tricky to determine when a C-section is necessary. The temperature and heart rate (both of the birthing person and of the fetus) can change quickly, and determining the size a baby will be at birth is not an absolute science. But beyond these medical measurements, bias plays a significant role in harming patients—especially Black and Indigenous patients—and their families every day in the U.S.
One student in attendance inquired about when, exactly, the disbelief of Black women’s pain begins. The answer for many patients is “long before birth.” Further, perhaps patients who don’t feel heard by their providers are more inclined to change providers more frequently, complicating the process of tracking their health information over time.
Another student identified social determinants of health as a probable contributor to this inequity, sharing that only around 10% of health outcomes are actually determined by health. The remaining 90% are determined by a patient’s economic stability, education access and quality, healthcare access and quality, neighborhood and built environment, and social community context.
Proposing solutions
To close out the seminar, the group moved on to brainstorming potential solutions for shrinking these gaps in care.
Course professor Amy Cohn, PhD, got the ball rolling: “I think we should get our mechanical engineering friends to build a device that can better capture the size of the baby so we stop doing C-sections we don’t need and stop putting women through delivering babies that aren’t going to fit.”
Diverse ideas followed:
- Lean into midwifery and doula care to overcome this lack of trust that can be present in many provider-patient relationships.
- Develop hospital-led group prenatal care programs “where women receive their education—breastfeeding classes, birthing classes, nutrition classes—together, which is shown to drastically reduce preterm birth” and reduce outcome disparities. This strategy also takes less time for the clinics and can be less expensive overall to administer.
- Reduce variance in physician bias by concretizing standards for determining whether a C-section is needed or not.
- Implement performance metrics/dashboards so providers can be compared to their colleagues through audit feedback.
- Transition away from epidurals and towards nitrous oxide, which better allows patients to feel when their bodies are ready to push (as opposed to relying on the provider telling them when to push).
- Create a “pain translator” that allows providers to feel the pain that a patient is feeling. To this, Ivy named the harmful stereotype that Black folks generally have higher pain tolerances, as well as the often unconscious reaction providers have to Black folks expressing their pain of viewing them as “narcotics-seeking.”
In conclusion, Ivy spoke to a room mostly comprising industrial and operations engineers and offered the following:
“I think that one of the things about healthcare that’s really important is that it’s very personal. Everyone of us is a patient, and so therefore, when we think about ‘How can I make this system better,’ you know…we may not all drive trucks, we may not all be able to operate manufacturing systems, but we are all patients. So how do we think about making this system delivery better? I think we have a lot to contribute from that perspective.”
— Written by Hannah Buck, CHEPS Staff