This week’s Providing Better Healthcare Through Systems Engineering seminar series welcomed Andrew M. Fine, MD, MPH to share his insight into using artificial intelligence (AI) as a tool to mitigate physician burnout. Students, faculty, staff, clinicians, and community members gathered to discuss both the potential and the risks of AI-supplemented healthcare.
Fine specializes in pediatric emergency medicine, innovating both children’s healthcare and public health at large. As a Senior Associate Physician in Pediatrics at the Boston Children’s Hospital, Fine has experienced firsthand the effects of provider burnout. He also serves as an Associate Professor in Pediatrics and Emergency Medicine at Harvard Medical School. In the classroom, he promotes the great interconnections between informatics, clinical care, and pediatric public health.
The emergency medicine documentation burden
Fine is committed to making pediatric emergency care safer and more efficient by revolutionizing the systems and procedures that govern the patients’ and providers’ day-to-day care. He shared his experience with developing methods to incorporate real-time epidemiology into clinical prediction models and modeling emergency department (ED) admissions.
Fine’s initial presentation focused on clinician burnout as it relates to the extensive documentation required in the ED. He shared a quote from a colleague: “If I didn’t have to document, I’d have the best job in the world.” After demonstrating the impact that documentation redundancy has on provider satisfaction, he described the particular interactions that require clinicians to reiterate the same patient “story” time and time again.
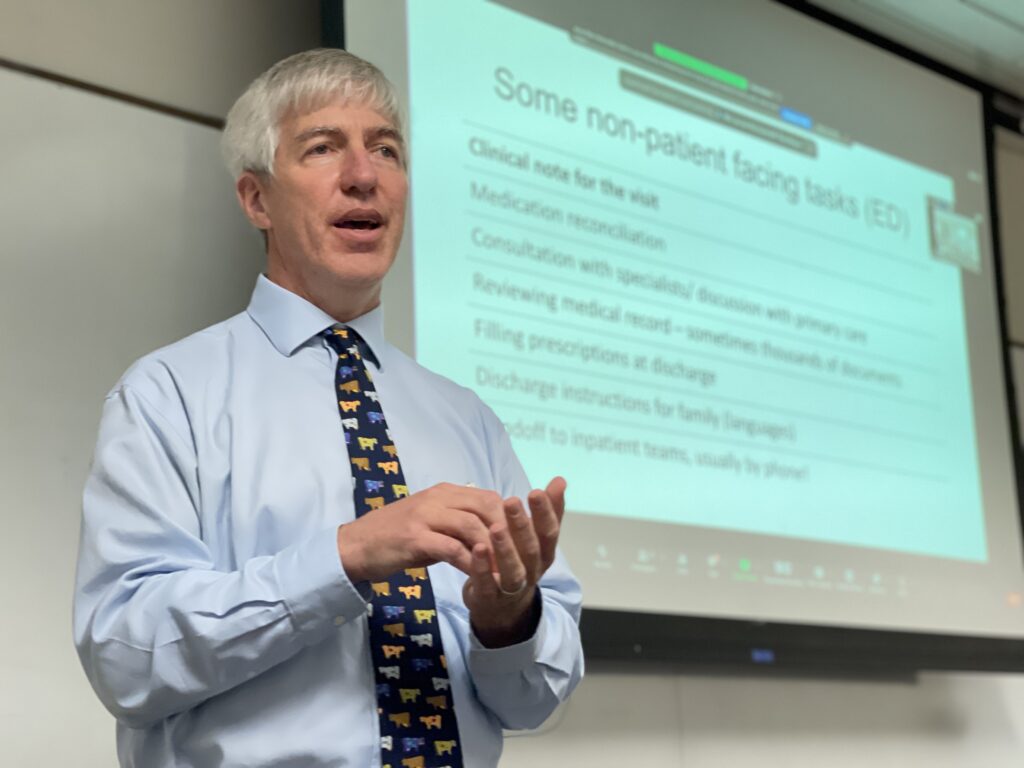
He began by shedding light on a few of the many non-patient-facing tasks that fall onto ED clinicians. From drafting a brief clinician summary of the appointment, extensive medication reconciliation, and medical record reviews, to providing discharge instructions for families and inpatient handoff specifications for further care, ED doctors have an immense task list to tackle for each and every patient.
He then provided two insightful statistics to really put this matter into perspective:
- Doctors are spending twice as much time documenting as they are actually interacting with and attending to their patients.
- In the last year, 50% of clinicians have experienced burnout.
Evidently, clinician burnout due to documentation is a potent and extensive issue in modern medicine…so what can we do?
Fine pivoted towards a discussion of artificial intelligence-based solutions with a quote from the American Medical Association president, Jesse Ehrenfeld: “It is clear to me that AI will never replace physicians – but physicians who use AI will replace those who don’t.” He shared several applications of AI to mitigate burnout that are of particular interest to researchers and developers. These included creating more efficient inpatient, discharge, and at-home care directions; automatically condensing more verbose, detail-oriented physician’s notes into more succinct clinician’s note summaries; and using AI to generate “IPASS” patient summary documents.

AI routes to condensing documentation
The seminar discussion focused particularly on how we could use technology to reduce the redundancy of documentation for ED clinicians. Fine kicked off the conversation by highlighting some major risks associated with automated healthcare including patient privacy, extended tasks for providers who have to “double-check” the output, and the all too common “hallucinations” (erroneous false information) that AI tools can generate.
Students shared ideas of using speech-to-text dictation, group messaging, and creating one centralized document to try and tackle this issue. One medical student spoke about a new “Start with a Draft” email workflow tool that the hospital is piloting with their team. This AI algorithm creates a response template for all the emails that the clinicians receive to steer the conversation in the right direction and reduce response time. The seminar attendees ran with this idea, suggesting a program that auto-generates a central document as the clinicians receive and input information. Another student suggested developing a program that can translate this document to best fit the recipient, whether that be a specialist, inpatient team, or family of the patient.
Join us
Join us on Monday, November 20th, for our much-awaited session with U-M IOE Department Chair Julie Simmons Ivy.
To RSVP to one or more sessions (or to request access to a session recording), please email [email protected]
— Written by Gabriel Ferriero, CHEPS Student