“We digitized U.S. healthcare . . . We are now trying to digitalize our workflow, and some is working well, and some is not.”
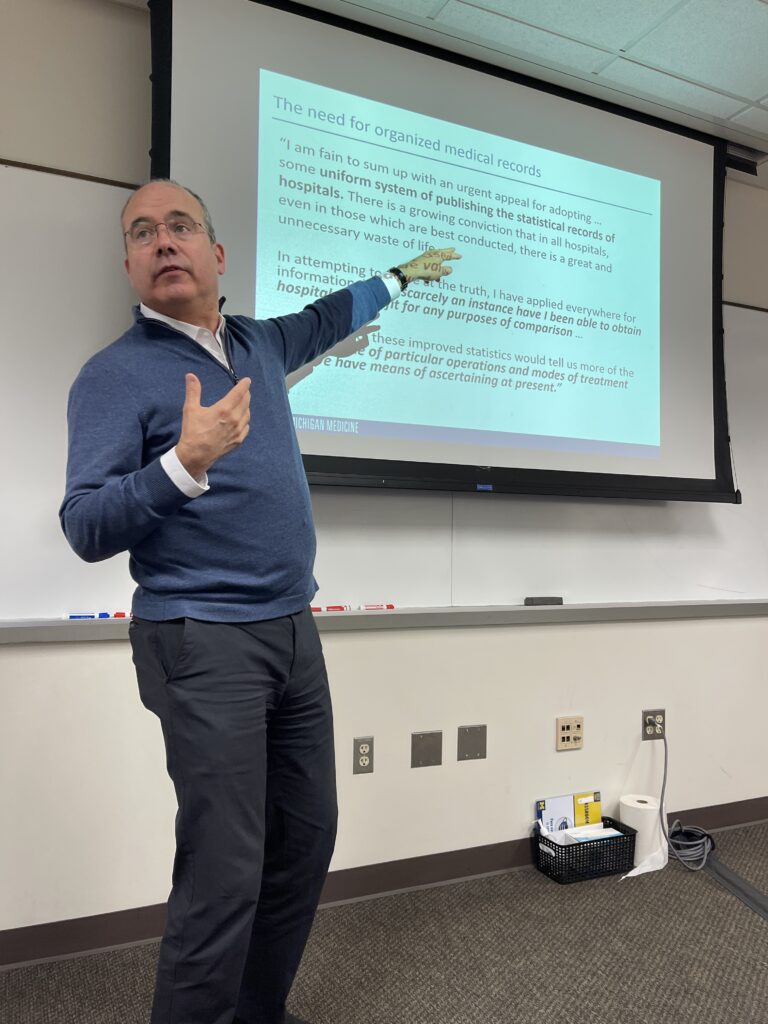
This is how Andrew Rosenberg, MD, Chief Information Officer of Michigan Medicine and Associate Professor of Anesthesiology and Internal Medicine, opened this week’s Providing Better Healthcare through Systems Engineering seminar session. His presentation, titled “Digitization-Digitalization-Digital Transformation: Changing Healthcare Paradigms” introduced students, faculty, staff, and community members from U-M and beyond to the complex reality that is adapting a centuries old profession—medicine—to the digital age.
Digitization, as Rosenberg described, refers to the creation of accessible digital infrastructure. One common example of digitization has been the move away from paper medical records to electronic health record systems. Digitalization, however, requires adapting existing systems and industries to effectively use these infrastructures.
“The work that we’ve done was mostly getting the rail gauges correct,” he shared, referring to the digitization that occurred largely throughout the 2000s and 2010s in the United States. “Now, the transformation can start—if we can figure out how to change our workflow.”
The digitization of healthcare has bettered the lives of many, allowing patients to request refills of their medicine with the tap of a finger, ensuring medical records don’t fall through the cracks between institutions of care, and empowering providers to help their patients from afar thanks to e-visits.
However, with technological gain can also come sacrifice.
Rosenberg provided an example that had been previously published in the Journal of the American Medical Association: a young child’s drawing depicting them and their family members visiting a doctor’s office. While each of the family members seem to be engaging with one another and smiling, the doctor is facing away from them all, seated at a computer and looking down while typing.

While typewritten notes allow for more detail to be recorded in a shorter amount of time, they also reduce the “face time” that patients get with their providers.
Similarly, contemporary pagers have been improved to not only beep—alerting a provider that they are needed, somewhere, for something, by someone—but to send specific messages, so providers can react to their patients’ needs more quickly and consistently than ever before. But what happens when a provider is already in an essential space? What happens when their pager sounds 45 times during rounds, an unskippable part of their job and an integral aspect of good patient care?
As Rosenberg posited, “Did we solve the problem, or did we create a new one? . . . If we adopt new technologies but we don’t fundamentally change workflow, we’re probably not going to make a real big difference.”
Enter digitalization.
Rosenberg sees opportunity for true digitalization to improve healthcare for patients and providers alike. Virtual reality, augmented reality, and mobile technology—when thoughtfully utilized to (re)build optimized systems and processes—hold great power, especially within the areas of precision health and artificial intelligence. Moore’s Law, Rosenberg adds, indicates that digital costs will decrease as time goes on, ultimately enabling widespread access and improved health outcomes across the country…and hopefully, the world.
Join us
We will reconvene on Monday, October 23rd with Michigan Medicine’s Medical Director of Interventional Nephrology and Vascular Access Services, Karthik Ramani. Join us then at 4:30 PM in IOE 1680.
To RSVP to one or more sessions (or to request access to a session recording), please email [email protected].
— Written by Hannah Buck, CHEPS Staff