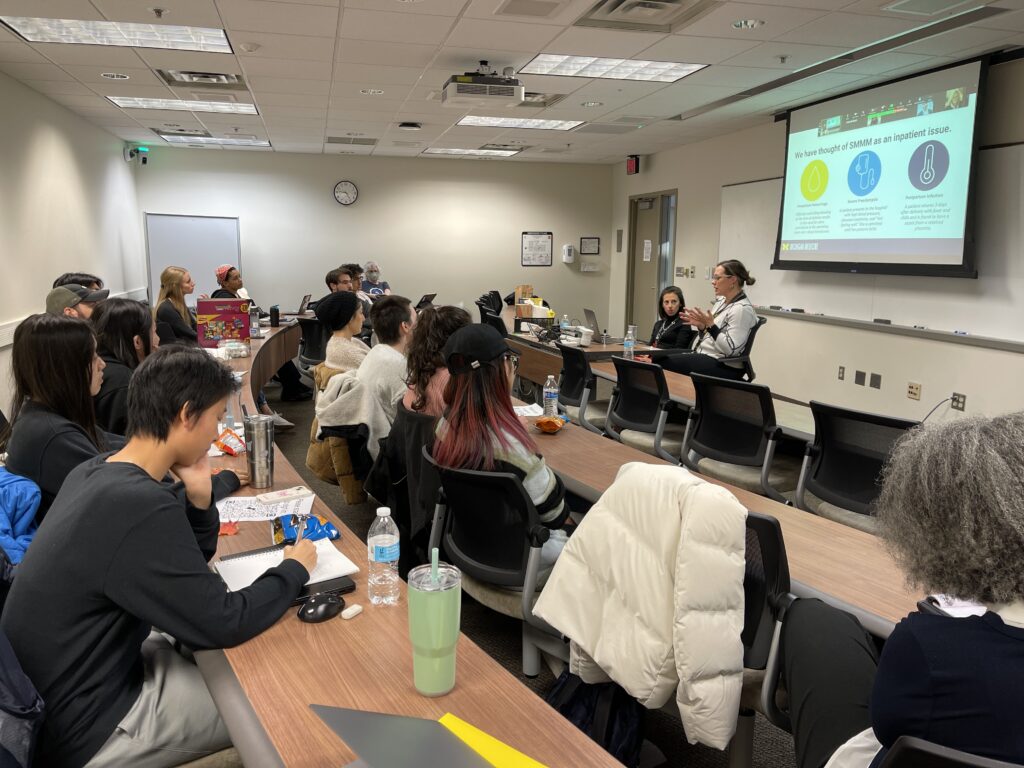
On October 30th, the Providing Better Healthcare through Systems Engineering seminar series had the privilege of hosting two distinguished speakers, Molly Stout, MD, MS and Alex Peahl, MD, MSc, who shed light on a critical topic: “Improving Access and Overcoming Barriers to Maternal Care Services.”
As a physician-scientist, Division Director of Maternal Fetal Medicine, and Associate Professor of Obstetrics and Gynecology at U-M, Stout shows great passion for optimizing prenatal care with an emphasis on those who need it most. Stout’s work is driven by a dedication to ensuring the well-being of birthing people and infants with the ultimate goal of making prenatal care accessible and effective for everyone.
Peahl is a physician and Assistant Professor of Obstetrics and Gynecology, as well as a health services researcher at U-M. Her research focuses on improving the effectiveness, efficiency, and equity of prenatal care through high-quality maternity care interventions. She has been collaborating with CHEPS for five years.
To ground the discussion, Stout began by revealing a startling statistic—over 80% of maternal deaths in the U.S. are preventable. This seminar asked attendees to question how data can be utilized to address severe maternal morbidity and mortality, as well as what the limits and impacts of those complex data-driven decisions are.
Next, Peahl introduced the “Goldilocks Dilemma” of prenatal care, highlighting the problem that some patients receive too much care (which can create financial, transportation, and social-emotional barriers to positive health outcomes) while others don’t receive enough. To address this dilemma, Peahl examined the conventional model of prenatal care. This traditional schedule requires more than 40 hours of care for a single patient, not accounting for social factors or additional care for complications. During the COVID-19 pandemic, however, many providers shifted to a more flexible approach. This model maintains all the essential services of the traditional model, but introduces greater flexibility by reducing the number of appointments and offering virtual care where reasonable.
While customized care is gaining traction across the country and the world, complex implementation considerations persist. These include the need to assess risk, accommodate patient preferences, and develop practical methods for monitoring patients. Over the past several years, the PATH (Prenatal Plan for Appropriate Tailored Healthcare) project at CHEPS has been actively addressing the challenge of risk stratification by creating a scoring system that evaluates a patient’s risk on a two-dimensional scale, considering both medical and psychological risk factors.
Although hurdles remain, tailored care that considers individuals’ social and medical factors has the potential to enhance the accessibility, efficiency, and equity of maternal care services.
Join us
Our next session will take place on Monday, November 13th at 4:30 PM. Join us then we we welcome Andrew Fine, MD, MPH, physican of Emergency Medicine at Boston Children’s Hospital and Associate Professor of Pediatrics at Harvard University. Spots available in person in IOE 1680 or online via Zoom.
To RSVP to one or more sessions (or to request access to a session recording), please email [email protected].
— Written by Mengting Tu, CHEPS Student